Keystone Flap for Reconstruction of Sacral and Ischial Pressure Injury
DOI:
https://doi.org/10.14228/jprjournal.v8i1.319Keywords:
Reconstruction of Sacral, Keystone Flap, Ischial Pressure InjuryAbstract
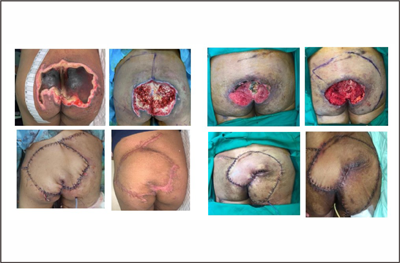
Introduction: Reconstruction of sacral and ischial pressure injury offers great challenges due to its high complication and recurrence rate. Providing durable tissue coverage with minimal donor site morbidity is paramount while ensuring fast operative time for the patients who often possess multiple comorbidities. This study aims to present cases of sacral and ischial pressure injury reconstruction using a keystone flap.
Method: A retrospective study was performed by reviewing data from fifteen patients with a sacral and ischial pressure injury who underwent reconstruction using various types of keystone flaps in our center between 2019 and 2020.
Results: The patients’ age ranged from 10 to 83 years old (average, 40.5 years old). The average wound dimensions were 9.4 ± 3.1 cm x 6.5 ± 2.7 cm and the mean area of the defects was 52.3 ± 35.7 cm2, with the largest defect was 15 x 12 cm (141.3 cm2). Mean operative time was 140 ± 24.5 minutes with nine wounds were reconstructed using type IV keystone flap (60%) and six patients using type IIA (40%). Postoperative complications occurred in three patients (20%). Other patients resulted in uneventful complete healing.
Conclusion: The keystone flap is reliable, simple, has a fast technique, and minimal donor site morbidity to cover the defects of sacral and ischial pressure injury. Performing thorough debridement, choosing the right type of keystone flap, elevating the flap adequately to allow mobilization, preserving perforator “hotspots”, and suturing of the flap without tension are keys to achieve satisfactory results.
References
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585.
Lyder CH. Pressure ulcer prevention and management. Jama. 2003;289(2):223-6.
Kottner J, Cuddigan J, Carville K, et al. Pressure ulcer/injury classification today: An international perspective. J Tissue Viability. 2020;29(3):197-203.
Zhou Q, Yu T, Liu Y, et al. The prevalence and specific characteristics of hospitalised pressure ulcer patients: A multicentre cross?sectional study. J Clin Nurs. 2018;27(3-4):694-704.
Padula WV, Pronovost PJ, Makic MB, et al. Value of hospital resources for effective pressure injury prevention: a cost-effectiveness analysis. BMJ Qual Saf. 2019;28(2):132-41.
Gillespie BM, Walker RM, Latimer SL, et al. Repositioning for pressure injury prevention in adults. Cochrane Database Syst Rev. 2020(6).
Dealey C, Posnett J, Walker A. The cost of pressure ulcers in the United Kingdom. J Wound Care. 2012;21(6):261-6.
Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil. 2000;81(12):1556-62.
Sørensen JL, Jørgensen B, Gottrup F. Surgical treatment of pressure ulcers. Am J Surg. 2004;188(1):42-51.
Chen YC, Huang EY, Lin PY. Comparison of gluteal perforator flaps and gluteal fasciocutaneous rotation flaps for reconstruction of sacral pressure sores. J Plast Reconstr Aesthet Surg. 2014;67(3):377-82.
Minami RT, Mills RO, Pardoe R. Gluteus maximus myocutaneous flaps for repair of pressure sores. Plast Reconstr Surg. 1977;60(2):242-9.
Sameem M, Au M, Wood T, Farrokhyar F, Mahoney J. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg. 2012;130(1):67e-77e.
Lee SS, Huang SH, Chen MC, Chang KP, Lai CS, Lin SD. Management of recurrent ischial pressure sore with gracilis muscle flap and VY profunda femoris artery perforator-based flap. J Plast Reconstr Aesthet Surg. 2009;62(10):1339-46.
Koshima I, Moriguchi T, Soeda S, Kawata S, Ohta S, Ikeda A. The gluteal perforator-based flap for repair of sacral pressure sores. Plast Reconstr Surg. 1993;91(4):678-83.
Borman H, Maral T. The gluteal fasciocutaneous rotation-advancement flap with VY closure in the management of sacral pressure sores. Plast Reconstr Surg. 2002;109(7):2325-9.
Byun IH, Kim CW, Park TH. The modified keystone flap for pressure ulcers: a modification of the keystone flap with rotation and advancement. Ann Plast Surg. 2019;82(3):299-303.
Coskunfirat OK, Özgentas HE. Gluteal perforator flaps for coverage of pressure sores at various locations. Plast Reconstr Surg. 2004;113(7):2012-7.
Lee JT, Hsiao HT, Tung KY, Ou SY. Gluteal perforator flaps for coverage of pressure sores at various locations. Plast Reconstr Surg. 2006;117(7):2507-8.
Hallock GG. The propeller flap version of the adductor muscle perforator flap for coverage of ischial or trochanteric pressure sores. Ann Plast Surg. 2006;56(5):540-2.
Lemaire V, Boulanger K, Heymans O. Free flaps for pressure sore coverage. Ann Plast Surg. 2008;60(6):631-4.
Yang CH, Kuo YR, Jeng SF, Lin PY. An ideal method for pressure sore reconstruction: a freestyle perforator-based flap. Ann Plast Surg. 2011;66(2):179-84.
Kim YS, Lew DH, Roh TS, Yoo WM, Lee WJ, Tark KC. Inferior gluteal artery perforator flap: a viable alternative for ischial pressure sores. J Plast Reconstr Aesthet Surg. 2009;62(10):1347-54.
Verpaele AM, Blondeel PN, Van Landuyt K, et al. The superior gluteal artery perforator flap: an additional tool in the treatment of sacral pressure sores. Br J Plast Surg. 1999;52(5):385-91.
Wettstein R, Tremp M, Baumberger M, Schaefer DJ, Kalbermatten DF. Local flap therapy for the treatment of pressure sore wounds. Int Wound J. 2015;12(5):572-6.
Lin CT, Chen SY, Chen SG, Tzeng YS, Chang SC. Parasacral perforator flaps for reconstruction of sacral pressure sores. Ann Plast Surg. 2015;75(1):62-5.
Akan IM, Sungur N, Özdemi R, Klnç H, Sensöz Ö. “Pac Man” flap for closure of pressure sores. Ann Plast Surg. 2001;46(4):421-5.
Kuo PJ, Chew KY, Kuo YR, Lin PY. Comparison of outcomes of pressure sore reconstructions among perforator flaps, perforator?based rotation fasciocutaneous flaps, and musculocutaneous flaps. Microsurgery. 2014;34(7):547-53.
Behan, FC. The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73(3):112-20.
Gómez OJ, Barón OI, Peñarredonda ML. Keystone Flap: Overcoming Paradigms. Plast Reconstr Surg Global Open. 2019;7(3).
Behan FC, Rozen WM, Lo CH, Findlay M. The omega - ? - variant designs (types A and B) of the keystone perforator island flap. ANZ J Surg. 2011;81:650–652.
Gupta S, Baharestani M, Baranoski S, et al. Guidelines for managing pressure ulcers with negative pressure wound therapy. Adv Skin Wound Care. 2004;17:1-6.
M?sl?man AM, Kar?ida? S, Sucu DÖ, et al. Clinical outcomes of myelomeningocele defect closure over 10 years. J Clin Neurosci. 2012;19:984-90.
Cheng H, Clymer JW, Chen BP, Sadeghirad B, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134-44.
Chih-Hsun L, Ma H. Use of perforator-based fasciocutaneous flaps for pressure sore reconstruction: Single-perforator-based versus multiple-perforator-based flaps. Aesthet Plast Surg. 2016;40(4):540-8.
Downloads
Published
Issue
Section
License
Copyright (c) 2021 Narottama Tunjung, Nandita Melati Putri

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors retain the copyright of the article and grant Jurnal Plastik Rekonstruksi the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License. Articles opting for open access will be immediately available and permanently free for everyone to read, download and share from the time of publication. All open access articles are published under the terms of the Creative Commons Attribution-Non-commercial-NoDerivatives (CC BY-NC-ND) which allows readers to disseminate and reuse the article, as well as share and reuse of the scientific material. It does not permit commercial exploitation or the creation of derivative works without specific permission.













