Results of Measuring Lactate Levels Value in Free Flap Reconstruction
DOI:
https://doi.org/10.25251/k4cg2w54Keywords:
Free flap monitoring method, vascular compromise, lactateAbstract
Introduction : Free flap surgery which is performed by transferring tissue along with its vascularization, can fail due to vascular compromised which cause by thrombosis formation either in vein or artery. Disruption of blood flow patency that not treated immediately can cause ischemia and necrosis occurred in free flap, especially within five days after reconstruction. Previous study has proven that free flap monitoring with lactate levels measurement can accurately for evaluate the occurrence vascular compromised in free flap.
Method : This study is a descriptive observational study with cross-sectional design. It was conducted by observing medical record of free flap reconstruction patient from November 2022 until November 2023 at Plastic and Reconstructive Surgery Department of RSUP Dr. Mohammad Hoesin Palembang. Data collection was carried out using total sampling technique and analysed using Statistical Package for the Social Science (SPSS) version 22.0 with univariate technique.
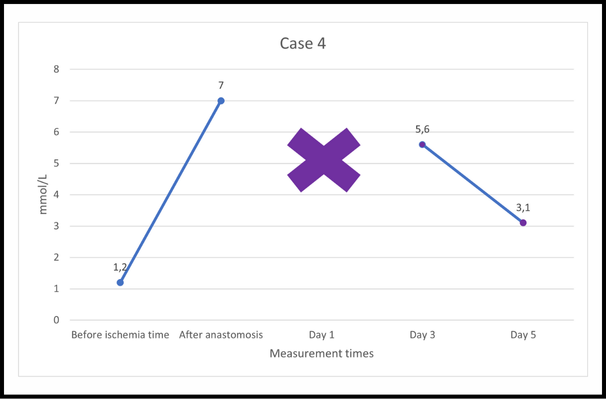
Result : Free flap with vascular compromise has higher lactate levels value than viable one. Lactate levels value transition of viable free flap showed an increase after anastomosis and gradually decrease at the next assessment time, while lactate levels in free flap with vascular compromise increased to above reference value, mainly on the first day vascular compromise occurred.
Conclusion: Clinical monitoring which combined with lactate levels assessment can accelerate the diagnose of blood flow patency disruption in free flap so that cause success rate improvement and better prognosis of free flap reconstruction patients.
References
Moosa S, Dydynsky R. The Role of Artificial Intelligence in Predicting Flap Outcomes in Plastic Surgery: Protocol of a Systematic Review. Undergrad Res Nat Clin Sci Technol URNCST J. 2022 May 4;1–8.
2. Kohlert S, Quimby A, Saman M, Ducic Y. Postoperative Free-Flap Monitoring Techniques. Semin Plast Surg. 2019 Feb;33(01):013–6.
3. Ritschl L, Schmidt L, Fichter A, Hapfelmeier A, Kanatas A, Wolff KD, et al. Prediction of Flap Necrosis by Using Indocyanine Green Videoangiography in Cases of Venous Occlusion in the Epigastric Flap Model of the Rat. J Reconstr Microsurg Open. 2018 Jul;03(02):e62–9.
4. David G, Vivien M, Sarra C, Brice G, Anna H, Philippe R, et al. Monitoring of myocutaneous flaps by intracapillary glucose and lactate measurements: experimental study. Clin Pract [Internet]. 2017 [cited 2023 Jul 24];14(2). Available from: http://www.openaccessjournals.com/articles/monitoring-of-myocutaneous-flaps-by-intracapillary-glucose-and-lactate-measurements-experimental-study.html
5. Birkenfeld F, Naujokat H, Helmers AK, Purcz N, Möller B, Wiltfang J. Microdialysis in postoperative monitoring of microvascular free flaps: Experiences with a decision algorithm. J Cranio-Maxillofac Surg. 2019 Aug;47(8):1306–9.
6. Karakawa R, Yoshimatsu H, Narushima M, Iida T. Ratio of Blood Glucose Level Change Measurement for Flap Monitoring. Plast Reconstr Surg - Glob Open. 2018 Jul;6(7):e1851.
7. Kishi K, Ishida K, Makino Y, Miyawaki T. A Simple Way to Measure Glucose and Lactate Values During Free Flap Head and Neck Reconstruction Surgery. J Oral Maxillofac Surg. 2019 Jan;77(1):226.e1-226.e9.
8. Kääriäinen M, Halme E, Laranne J. Modern postoperative monitoring of free flaps. Curr Opin Otolaryngol Head Neck Surg. 2018 Aug;26(4):248–53.
9. Tachi K, Nakatsukasa S, Nakayama Y. Monitoring free flap venous congestion using continuous tissue glucose monitoring: A case report. JPRAS Open. 2018 Sep;17:49–53.
10. Handayani S. A Simple Method to Measure Serum Lactate Concentration as A Reliable Parameter to Detect Flaps Blood-flow Patency. J Plast Rekonstr [Internet]. 2012 [cited 2023 Jul 24];1(4). Available from: http://jprjournal.com/index.php/jpr/article/view/89
11. Henault B, Pluvy I, Pauchot J, Sinna R, Labruère-Chazal C, Zwetyenga N. Capillary measurement of lactate and glucose for free flap monitoring. Ann Chir Plast Esthét. 2014 Feb;59(1):15–21.
12. Nikhar SA, Metta R, Nimmagadda R, Gopinath R. Does the systemic rise in serum lactate levels correlate to free flap failure in head and neck reconstructive surgeries—series of cases. Ain-Shams J Anesthesiol. 2023 Sep 12;15(1):73.
13. Rabinowitz JD, Enerbäck S. Lactate: the ugly duckling of energy metabolism. Nat Metab. 2020 Jul;2(7):566–71.
14. Setala L, Gudaviciene D. Glucose and Lactate Metabolism in Well-Perfused and Compromised Microvascular Flaps. J Reconstr Microsurg. 2013 Jun 11;29(08):505–10.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Mufida Muzakkie, Karnissa Rizkia Adhania

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors retain the copyright of the article and grant Jurnal Plastik Rekonstruksi the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License. Articles opting for open access will be immediately available and permanently free for everyone to read, download and share from the time of publication. All open access articles are published under the terms of the Creative Commons Attribution-Non-commercial-NoDerivatives (CC BY-NC-ND) which allows readers to disseminate and reuse the article, as well as share and reuse of the scientific material. It does not permit commercial exploitation or the creation of derivative works without specific permission.













